Neglected Global Diseases
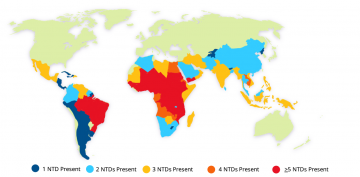
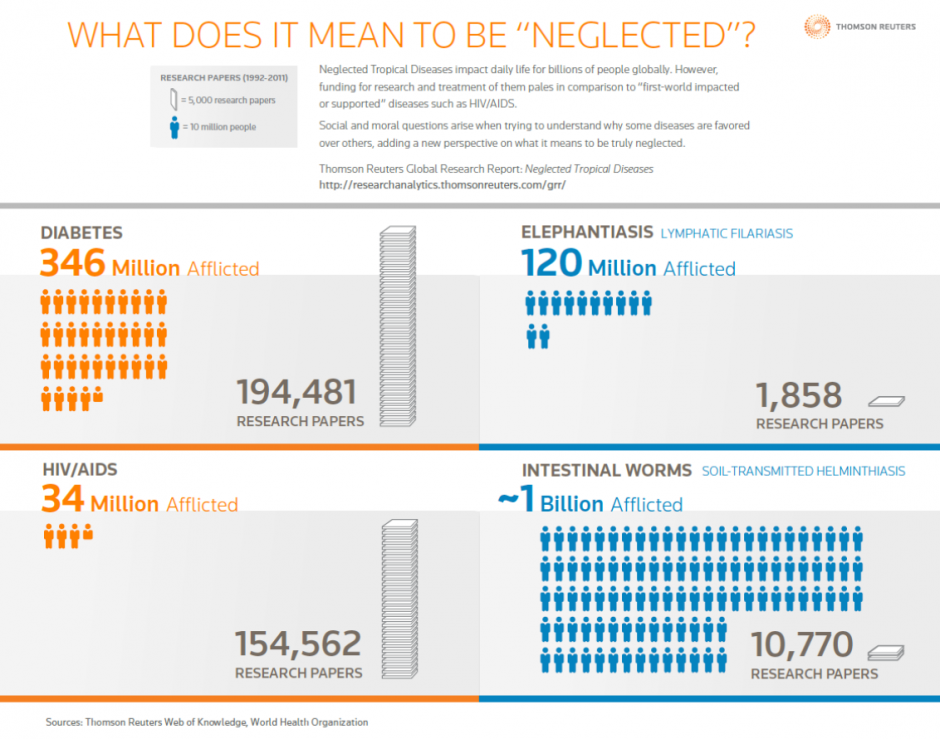
Neglected Global Diseases (NGDs) are infectious diseases and other conditions that cause physical and cognitive impairments, contribute to mother and child illness and death, and make it difficult to earn a living, thereby disproportionately affecting the world’s poorest populations. They include maternal, infant and child health conditions, neglected tropical diseases (NTDs) as well as HIV/AIDS, tuberculosis, and malaria. The World Health Organization (WHO) has a list of 18 NTDs that, combined, causes substantial illness for more than one billion people globally (see image on the right). These diseases thrive in conditions of extreme poverty; areas that generally have unsafe water, poor sanitation, substandard housing, and limited access to health care or essential medicines. In some countries this includes most rural areas, urban slums, or conflict zones, however, it is increasingly recognized that emerging middle-income countries (Brazil, Russia, India, China, and South Africa) contain the highest numbers of people affected.
NGDs impact daily life for billions of people globally. In countries with weak health and social support systems, they cripple families and contribute to the harsh cycle of poverty. While some NTDs are fatal without treatment, most of them are debilitating and stigmatizing. Children are particularly vulnerable. Overall, NGDs cause great suffering and are a leading cause of chronic disability, diminished quality of life, and premature death. Despite their impact, funding for NTDs research and treatment pales in comparison to “first-world impacted or supported diseases.” The social and moral question that must be asked is, “why are these diseases, that effect billions of people, neglected?”
Neglected Tropical Diseases
The following information is from the WHO fact sheets on NTDs (used by permission).
Buruli ulcer is a chronic debilitating skin and soft tissue infection that can lead to permanent disfigurement and disability. It is caused by the Mycobacterium ulcerans bacertium. At least 33 countries with tropical, subtropical, and temperate climates have reported Buruli ulcer, with 5000-6000 cases annually reported from 15 of the countries. The majority of infections are found in rural communities in sub-Saharan Africa. Nearly half of those affected in Africa are children under the age of 15yrs. Early detection is vital as ~80% of early cases can be cured with a combination of antibiotics.
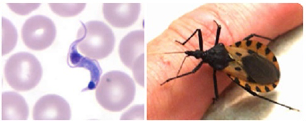 About 7 million to 8 million people worldwide are estimated to be infected with Trypanosoma cruzi (the parasite that causes Chagas disease) worldwide, mostly in Latin America. Chagas disease was once entirely confined to the Region of the Americas – principally Latin America – but it has now spread to other continents. Chagas disease is curable if treatment is initiated soon after infection. Up to 30% of chronically infected people develop cardiac alterations and up to 10% develop digestive, neurological or mixed alterations, for which specific treatment may become necessary. Vector control is the most useful method to prevent Chagas disease in Latin America. Blood screening is vital to prevent infection through transfusion and organ transplantation.
About 7 million to 8 million people worldwide are estimated to be infected with Trypanosoma cruzi (the parasite that causes Chagas disease) worldwide, mostly in Latin America. Chagas disease was once entirely confined to the Region of the Americas – principally Latin America – but it has now spread to other continents. Chagas disease is curable if treatment is initiated soon after infection. Up to 30% of chronically infected people develop cardiac alterations and up to 10% develop digestive, neurological or mixed alterations, for which specific treatment may become necessary. Vector control is the most useful method to prevent Chagas disease in Latin America. Blood screening is vital to prevent infection through transfusion and organ transplantation.
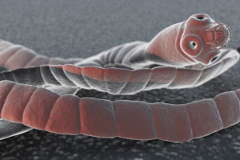 Cysticercosis/Taeniasis is an intestinal infection caused through the inadvertent ingestion of tapeworm larval cysts (cysticerci) in undercooked pork or beef. Three parasite species cause taeniasis in humans, T. solium (pork tapeworm), T. saginata (beef tapeworm), and T. asiatica. Human tapeworm carriers contaminate the environment with tapeworm eggs which pass out with feces. Humans can also become infected with T. solium eggs due to poor hygiene. Cysticercosis can be devastating to human health. It is the infection of tissues caused by larvae (cysticerci) as a result of ingesting T. solium eggs. Cysts that develop in the central nervous system cause neurocysticercosis – the most severe form of the disease and one of the main preventable causes of epilepsy (seizures) in many developing countries. More than 80% of the world’s 50 million people who are affected by epilepsy live in low-income and lower-middle-income countries, many of which are endemic for T. solium infections in people and pigs.
Cysticercosis/Taeniasis is an intestinal infection caused through the inadvertent ingestion of tapeworm larval cysts (cysticerci) in undercooked pork or beef. Three parasite species cause taeniasis in humans, T. solium (pork tapeworm), T. saginata (beef tapeworm), and T. asiatica. Human tapeworm carriers contaminate the environment with tapeworm eggs which pass out with feces. Humans can also become infected with T. solium eggs due to poor hygiene. Cysticercosis can be devastating to human health. It is the infection of tissues caused by larvae (cysticerci) as a result of ingesting T. solium eggs. Cysts that develop in the central nervous system cause neurocysticercosis – the most severe form of the disease and one of the main preventable causes of epilepsy (seizures) in many developing countries. More than 80% of the world’s 50 million people who are affected by epilepsy live in low-income and lower-middle-income countries, many of which are endemic for T. solium infections in people and pigs.
 Dengue is a mosquito-borne viral infection. The infection causes flu-like illness, and occasionally develops into a potentially lethal complication called severe dengue. The global incidence of dengue has grown dramatically in recent decades with about half of the world's population is now at risk. Dengue is found in tropical and sub-tropical climates worldwide, mostly in urban and semi-urban areas. Severe dengue is a leading cause of serious illness and death among children in some Asian and Latin American countries. There is no specific treatment for dengue/ severe dengue, but early detection and access to proper medical care lowers fatality rates below 1%. Dengue prevention and control solely depends on effective vector control measures.
Dengue is a mosquito-borne viral infection. The infection causes flu-like illness, and occasionally develops into a potentially lethal complication called severe dengue. The global incidence of dengue has grown dramatically in recent decades with about half of the world's population is now at risk. Dengue is found in tropical and sub-tropical climates worldwide, mostly in urban and semi-urban areas. Severe dengue is a leading cause of serious illness and death among children in some Asian and Latin American countries. There is no specific treatment for dengue/ severe dengue, but early detection and access to proper medical care lowers fatality rates below 1%. Dengue prevention and control solely depends on effective vector control measures.
 Dracunculiasis (guinea-worm disease) is a crippling parasitic disease on verge of eradication, with only 54 cases reported in 2019. The parasite is transmitted when people drink stagnant water contaminated with parasite-infected water-fleas (cyclops). From the time infection occurs, it takes between 10-14 months for the cycle to complete until a mature worm emerges from the body. Of the 20 countries that were endemic in the mid 1980s, only 4 (all on the African continent) reported cases in 2019: Angola (1 case), Chad (48 cases), South Sudan (4 cases) and Cameroon (1 case, likely imported from Chad).
Dracunculiasis (guinea-worm disease) is a crippling parasitic disease on verge of eradication, with only 54 cases reported in 2019. The parasite is transmitted when people drink stagnant water contaminated with parasite-infected water-fleas (cyclops). From the time infection occurs, it takes between 10-14 months for the cycle to complete until a mature worm emerges from the body. Of the 20 countries that were endemic in the mid 1980s, only 4 (all on the African continent) reported cases in 2019: Angola (1 case), Chad (48 cases), South Sudan (4 cases) and Cameroon (1 case, likely imported from Chad).
 Human echinococcosis is a parasitic disease caused by tapeworms of the genus Echinococcus. The two most important forms of the disease in humans are cystic echinococcosis (hydatidosis) and alveolar echinococcosis. Humans are infected through ingestion of parasite eggs in contaminated food, water or soil, or after direct contact with animal hosts. Echinococcosis is often expensive and complicated to treat and may require extensive surgery and/or prolonged drug therapy. Prevention programmes involve deworming of dogs, improved slaughterhouse hygiene, and public education campaigns; vaccination of lambs is currently being evaluated as an additional intervention. WHO is working towards the validation of effective cystic echinococcosis control strategies by 2018.
Human echinococcosis is a parasitic disease caused by tapeworms of the genus Echinococcus. The two most important forms of the disease in humans are cystic echinococcosis (hydatidosis) and alveolar echinococcosis. Humans are infected through ingestion of parasite eggs in contaminated food, water or soil, or after direct contact with animal hosts. Echinococcosis is often expensive and complicated to treat and may require extensive surgery and/or prolonged drug therapy. Prevention programmes involve deworming of dogs, improved slaughterhouse hygiene, and public education campaigns; vaccination of lambs is currently being evaluated as an additional intervention. WHO is working towards the validation of effective cystic echinococcosis control strategies by 2018.
 At least 56 million people globally suffer from one or more foodborne trematodiases. People become infected through the consumption of raw fish, crustaceans or vegetables that harbour the parasite larvae. Foodborne trematodiases are most prevalent in South-East Asia and South America. Foodborne trematodiases result in severe liver and lung disease. Safe and effective medicines are available to prevent and treat foodborne trematodiases.
At least 56 million people globally suffer from one or more foodborne trematodiases. People become infected through the consumption of raw fish, crustaceans or vegetables that harbour the parasite larvae. Foodborne trematodiases are most prevalent in South-East Asia and South America. Foodborne trematodiases result in severe liver and lung disease. Safe and effective medicines are available to prevent and treat foodborne trematodiases.
 Human African Trypanosomiasis (sleeping sickness) is an endemic in 36 sub-Saharan Africa countries where there are tsetse flies that transmit the disease. The disease is considered fatal without treatment. Those who are most exposed to the testse flies live in rural areas and depend on agriculture, fishing, animal husbandry or hunting for food. Diagnosis and treatment of the disease is complex and requires specifically skilled staff. There are 2 forms of sleeping sickness, depending on the parasite involved: Trypanosoma brucei gambiense accounts for more than 98% of reported cases. Sustained control efforts have lowered the number of new cases reported. In 2009, for the first time in 50 years, cases dropped below 10 000, and as of 2018, only 977 cases are recorded.
Human African Trypanosomiasis (sleeping sickness) is an endemic in 36 sub-Saharan Africa countries where there are tsetse flies that transmit the disease. The disease is considered fatal without treatment. Those who are most exposed to the testse flies live in rural areas and depend on agriculture, fishing, animal husbandry or hunting for food. Diagnosis and treatment of the disease is complex and requires specifically skilled staff. There are 2 forms of sleeping sickness, depending on the parasite involved: Trypanosoma brucei gambiense accounts for more than 98% of reported cases. Sustained control efforts have lowered the number of new cases reported. In 2009, for the first time in 50 years, cases dropped below 10 000, and as of 2018, only 977 cases are recorded.
 Leishmaniases are a group of diseases caused by protozoan parasites from more than 20 Leishmania species and transmitted by the bite of infected sandflies. There are several different forms of leishmaniasis in people, the most common are cutaneous leishmaniasis, which causes skin sores, and visceral leishmaniasis, which affects several internal organs (usually spleen, liver, and bone marrow). The disease is found in people in focal areas on every continent except Australia and Antarctica, especially in parts of the tropics, subtopics, and southern Europe. Leishmaniasis is linked to environmental changes such as deforestation, building of dams, irrigation schemes and urbanization. An estimated 1.3 million new cases and 20 000 to 30 000 deaths occur annually.
Leishmaniases are a group of diseases caused by protozoan parasites from more than 20 Leishmania species and transmitted by the bite of infected sandflies. There are several different forms of leishmaniasis in people, the most common are cutaneous leishmaniasis, which causes skin sores, and visceral leishmaniasis, which affects several internal organs (usually spleen, liver, and bone marrow). The disease is found in people in focal areas on every continent except Australia and Antarctica, especially in parts of the tropics, subtopics, and southern Europe. Leishmaniasis is linked to environmental changes such as deforestation, building of dams, irrigation schemes and urbanization. An estimated 1.3 million new cases and 20 000 to 30 000 deaths occur annually.
 Leprosy (aka Hansen’s disease) is an infection caused by slow-growing bacteria called Mycobacterium leprae. Incubation period of the disease is about 5 years and may take up to 20 years to develop signs of the infection. Leprosy affects the nerves, skin, eyes, and lining of the nose (nasal mucosa). It is not known how Leprosy spreads between people. Scientists currently think it is transmitted via droplets when a person with the disease coughs or sneezes, and a healthy person breathes in the droplets containing the bacteria. Once feared as a highly contagious and devastating disease, now with early diagnosis and treatment, leprosy is curable. Early diagnosis and treatment with multidrug therapy (MDT) remain key in eliminating the disease as a public health concern. If left untreated, the nerve damage can result in crippling of hands and feet, paralysis, and blindness.
Leprosy (aka Hansen’s disease) is an infection caused by slow-growing bacteria called Mycobacterium leprae. Incubation period of the disease is about 5 years and may take up to 20 years to develop signs of the infection. Leprosy affects the nerves, skin, eyes, and lining of the nose (nasal mucosa). It is not known how Leprosy spreads between people. Scientists currently think it is transmitted via droplets when a person with the disease coughs or sneezes, and a healthy person breathes in the droplets containing the bacteria. Once feared as a highly contagious and devastating disease, now with early diagnosis and treatment, leprosy is curable. Early diagnosis and treatment with multidrug therapy (MDT) remain key in eliminating the disease as a public health concern. If left untreated, the nerve damage can result in crippling of hands and feet, paralysis, and blindness.
 Lymphatic filariasis, commonly known as elephantiasis, affects over 120 million people in 72 countries throughout the tropics and sub-tropics of Asia, Africa, the Western Pacific, and parts of the Caribbean and South America. Lymphatic filariasis is a painful and profoundly disfiguring disease. The disease is caused by three species of thread-like nematode worms that form “nests” in the human lymphatic system, an essential component of the body’s immune system. Acute episodes of local inflammation involving the skin, lymph nodes and lymphatic vessels often accompany chronic lymphoedema. To interrupt transmission WHO recommends an annual mass drug administration of single doses of two medicines to all eligible people in endemic areas.
Lymphatic filariasis, commonly known as elephantiasis, affects over 120 million people in 72 countries throughout the tropics and sub-tropics of Asia, Africa, the Western Pacific, and parts of the Caribbean and South America. Lymphatic filariasis is a painful and profoundly disfiguring disease. The disease is caused by three species of thread-like nematode worms that form “nests” in the human lymphatic system, an essential component of the body’s immune system. Acute episodes of local inflammation involving the skin, lymph nodes and lymphatic vessels often accompany chronic lymphoedema. To interrupt transmission WHO recommends an annual mass drug administration of single doses of two medicines to all eligible people in endemic areas.
 Onchocerciasis or “river blindness is caused by the parasitic worm Onchocerca volvulus. It is transmitted to humans through exposure to repeated bites of infected blackflies of the genus Simulium. Symptoms include severe itching, disfiguring skin conditions and visual impairment, including permanent blindness. More than 99% of infected people infected live in sub-Saharan Africa; the disease also exists in some foci in Latin America and Yemen. Community-directed treatment with ivermectin is the core strategy to eliminate onchocerciasis in Africa; in the Americas the strategy is biannual large-scale treatment with ivermectin. As of 2020, 1.8 million people live in areas that no longer require mass drug administration for onchocerciasis.
Onchocerciasis or “river blindness is caused by the parasitic worm Onchocerca volvulus. It is transmitted to humans through exposure to repeated bites of infected blackflies of the genus Simulium. Symptoms include severe itching, disfiguring skin conditions and visual impairment, including permanent blindness. More than 99% of infected people infected live in sub-Saharan Africa; the disease also exists in some foci in Latin America and Yemen. Community-directed treatment with ivermectin is the core strategy to eliminate onchocerciasis in Africa; in the Americas the strategy is biannual large-scale treatment with ivermectin. As of 2020, 1.8 million people live in areas that no longer require mass drug administration for onchocerciasis.
Rabies occurs in more than 150 countries and territories. More than 55 000 people die of rabies every year mostly in Asia and Africa. 40% of people who are bitten by suspect rabid animals are children under 15 years of age. Dogs are the source of the vast majority of human rabies deaths. Wound cleansing and immunization within a few hours after contact with a suspect rabid animal can prevent the onset of rabies and death. Every year, more than 15 million people worldwide receive a post-exposure vaccination to prevent the disease– this is estimated to prevent hundreds of thousands of rabies deaths annually.
Schistosomiasis is a chronic disease caused by parasitic worms. At least 243 million people required treatment for schistosomiasis in 2011. The number of people reported to have been treated for schistosomiasis in 2011 was 28.1 million. People are at risk of infection due to agricultural, domestic and recreational activities which expose them to infested water. Lack of hygiene and play habits make children especially vulnerable to infection. Clean drinking water, adequate sanitation and hygiene education would reduce infective water contact and the contamination of water sources. Schistosomiasis control focuses on reducing disease through periodic, large-scale population treatment with praziquantel.
Soil-transmitted helminth infections are caused by different species of parasitic worms. They are transmitted by eggs present in human faeces, which contaminate the soil in areas where sanitation is poor. Approximately two billion people are infected with soil-transmitted helminths worldwide. Infected children are physically, nutritionally and cognitively impaired. Safe and effective medicines are available to control infection. Control is based on: periodical deworming to eliminate infecting worms; health education to prevent reinfection; and improved sanitation to reduce soil contamination with infective eggs.
Though the exact number of snake bites is unknown an estimated 5 million people are bitten each year with up to 2.5 million envenomings. At least 100 000 people die as a result of snake bites each year, and around three times as many amputations and other permanent disabilities are caused by snakebites annually. Bites by venomous snakes can cause paralysis that may prevent breathing; bleeding disorders that can lead to a fatal haemorrhage; irreversible kidney failure and tissue damage that can cause permanent disability and which may result in limb amputation. Agricultural workers and children are the most affected. Children often suffer more severe effects than adults, due to their smaller body mass.
Trachoma is estimated to be endemic in 53 countries and is responsible for the visual impairment of about 2.2 million people, of whom 1.2 million are irreversibly blind. Approximately 228,9 million people live in trachoma endemic areas and are at risk of infection. An estimated 47 million were treated with antibiotics in 2012 and 169 thousand received surgical treatment. Infection spreads through personal contact (hands, clothing) and by flies that have been in contact with discharge from the eyes and nose of infected persons. If left untreated, infection causes chronic sequelae with pain and discomfort and permanently damages the cornea of the eye, leading to irreversible blindness.
Yaws is a neglected tropical disease that affects the skin, bone and cartilage. The disease is caused by a bacterium from the same group of organisms that cause venereal syphilis; however, the transmission of yaws is not sexually-related. Yaws can be eradicated as humans are the only reservoir. A recent finding has shown that that a single, oral dose of the antibiotic azithromycin can completely cure yaws, opening up prospects for large-scale treatment of affected populations. 2 countries - Ecuador and India - which were once endemic reported interruption of transmission in 2003. 12 currently endemic countries need support to implement WHO’s new eradication strategy.
What is UBC doing to help?
At the University of British Columbia (UBC), there are a number of experts and groups leading studies that address neglected global diseases. The delivery of interventions for global health is a complex and interconnected activity. In order for new medications to reach those in need integrated research encompassing bench science, biotechnology, pharmaceutical and health research, business, social policy, economics and law and others is needed. Social determinants of health and implementation science are becoming increasingly recognized as providing critical information to the complex relationships affecting delivery.
UBC has developed an intellectual property initiative that harnesses the economic potential of university innovations (such as medical discoveries) to ensure their development, while at the same time enhancing their social benefit by ensuring reasonable, fair, and affordable access for developing countries. The Global Access Initiative is the first of its kind in Canadian Universities and was initially brought forth by a group of committed students from the UBC chapter of Universities Allied for Essential Medicines.
The Neglected Global Diseases Initiative at UBC provides a mechanism for interaction between these various groups in order to more effectively impact its neglected disease research outcomes. It is creating a network to bring together these groups and provide a foundation for developing continuity of funding–enhancing the impact and outcomes of research and enabling sustained scholarly activity and education in this area. The aim of the initiative is to bring together the technical expertise and perspective of a variety of disciplines to investigate innovative and effective ways of identifying and overcoming barriers to the successful generation of affordable, life-sustaining medicines for developing countries.
The pursuit of developing new drugs, nano-medicines, vaccines, therapeutics, diagnostics, micronutrients and prophylactic measures is already underway and research clusters are being formed by disease and platform to facilitate communication linkages. This UBC initiative stands apart from most others by its ability to present a cohesive approach from conception of the interventions to the final use in afflicted individuals.